KEY FINDINGS
- Unhealthy lifestyle habits can negatively affect cardiopulmonary parameters and contribute to respiratory muscle weakness.
- This case presents a 47-year-old female with impaired pulmonary function and elevated cardiovascular risk.
- Two weeks of respiratory muscle training improved pulmonary function, estimated lung age, and vascular elasticity and compliance.
- The findings highlight the effectiveness of RMT to slow cardiopulmonary decline and to reduce the risk of cardiovascular disease.
ABSTRACT
This case study highlights the usefulness of respiratory muscle training (RMT) in improving pulmonary and cardiovascular parameters as an early intervention to cardiopulmonary decline. We suggest RMT as an easily accessible, cost- and time-effective opportunity to support a healthy lifestyle.
Many lifestyle and occupational habits negatively impact physical and mental health, increasing the risk of cardiovascular and other diseases. While larger institutions fulfill occupational health requirements to ensure their employees’ wellbeing at work, smaller business workers and entrepreneurs may neglect initial signs of stress or physical decline, putting themselves at increased risk. Early detection of compromised cardiopulmonary health or fitness has the potential to flag up indications for early interventions and reduce the risk of disease onset and progression.
INTRODUCTION
A dysfunctional work-life balance, unhealthy lifestyle and unsupportive office culture, often in combination with a predominantly sedentary occupation, greatly contribute to the development of cardiopulmonary and cardiovascular conditions, setting the stage for a downward spiral until healthy habits are restored. Early detection of physiological changes at the beginning of the spiral has the potential to highlight increased risks before the onset of symptoms and disease. In addition, early, non-pharmacological countermeasures that can easily be integrated into a corporate lifestyle may be able to reverse those initial physiological changes, thereby reducing the risk of cardiovascular and cardiopulmonary disease.
This case report discusses findings from a 47-year-old successful corporate business owner with a suspected compromised diaphragm, mild restrictive lung disease, and reduced arterial elasticity. Strengthening of the respiratory muscles by inspiratory and expiratory muscle training improved pulmonary function and arterial compliance, potentially reducing the cardiovascular risk.
PATIENT
A 47-year-old female presented with shortness of breath (dyspnea) and fatigue following a diagnosis of mild restrictive lung disease, elevated cholesterol levels, and borderline hyperglycemia. The business owner had a self-reported predominantly sedentary lifestyle, with no exercise or rehabilitative activities prior to the intervention. She was a non-smoker with a BMI of 26.51 kg/m2 and adhered to soy- and gluten-free vegetarian diet. She did not report sleep disturbances or documented sleep apnea.
BASELINE AND FINAL ASSESSMENT
Before and after the intervention, the subject underwent a pulmonary function test using the MIR MiniSpir II PC Based Spirometer. Parameters assessed include forced expiratory volume (FEV1), forced vital capacity (FVC), peak expiratory flow (PEF), and an estimated lung age (ELA).
Arterial health was assessed using Max Pulse (Medicore). This device uses photoplethysmography to optically detect blood volume changes in the microvascular bed of tissue. This is achieved by measuring small variations in light intensity through the skin, reflecting differences in diffusion of the captured area. The peripheral pulse normally describes a waveform, synchronized with the heartbeat. Changes in the synchronization are characteristic of changes in endothelial stiffness and flow resistance, indicating an increase in early cardiovascular risk factors. The device also assesses heart rate and heart rate variability.
INTERVENTION
After the baseline assessment, the patient was introduced to the Breather®️ (PN Medical, Inc.), a respiratory muscle training (RMT) device. The device activates inspiratory as well as expiratory muscle groups by providing adjustable resistance to the airflow during inhalation and exhalation. Resistance settings for each part of the breath cycle can be set independently of each other, providing the opportunity to train each muscle group at the intended target effort.
The patient was instructed to perform RMT twice a day, every day, doing 2 sets of 10 breaths, at moderate to a somewhat hard effort (70% to 80% of maximum effort). The patient followed the RMT protocol for 17 days, with self-reported compliance of 100% for the duration of the intervention.
The patient was not started on new medications or changed her diet, lifestyle or exercise routine during the duration of the intervention.
RESULTS AND DISCUSSION
Table 1 provides an overview of the results obtained from the baseline and final assessment of the patient, outlining the observed changes.
| Biomarker | Pre | Post | Change |
| Arterial Elasticity | 48 | 53 | 10.4% |
| Peripheral Elasticity | 51 | 95 | 86.3% |
| Differential Pulse Index | 3 | 2 | N/A |
| FVC (l) | 2.67 | 2.90 | 0.23(8.6%) |
| FVC (% predicted) | 80 | 87 | 7% |
| FEV1 (l) | 2.14 | 2.33 | 0.19(8.9%) |
| FEV1 (% predicted) | 80 | 87 | 7% |
| PEF (l/s) | 5.56 | 6.12 | 0.56(10.1%) |
| PEF (%predicted) | 86 | 94 | 8% |
| Estimated Lung Age | 67 | 61 | 6 years |
Table 1: Pulmonary and cardiovascular assessments before (pre) and after (post) RMT intervention (17 days). The change indicates the differences observed between the baseline and end-line assessments.
EFFECT OF RMT ON PULMONARY FUNCTION
Assessment of pulmonary function shows that the RMT intervention improves both the forced vital capacity as well as forced expiratory volume, indicating a partial reversal in the restrictive impairment causing the symptoms of dyspnea and fatigue. Due to the nature of the study, it is not possible to exclude the possibilities of fluctuations inherent to the measuring method, or more effective technique during the assessment to be responsible for the observed improvements.
Improvements in these pulmonary parameters result in a decrease in estimated lung age by 6 years, reducing the gap between ELA and the chronological age of the patient (47). Although respiratory muscle strength was not directly evaluated by maximum inspiratory or expiratory pressure (MIP/MEP), a strengthening effect of the intervention can be assumed based on the self-reported high compliance to the training protocol and the improved pulmonary parameters assessed by PFT (FVC, FEV1, and PEF, see table 1), as well as on established improvements in respiratory muscle strength reported elsewhere [1].
These findings are in line with reports showing that RMT improves pulmonary function, dyspnea, exercise tolerance, and fatigue in patients with restrictive lung disease [2]. Based on these observations, it is reasonable to presume that the patient’s pulmonary function improved due to the RMT intervention, potentially contributing to a positive impact on the restrictive lung condition and associated symptoms.
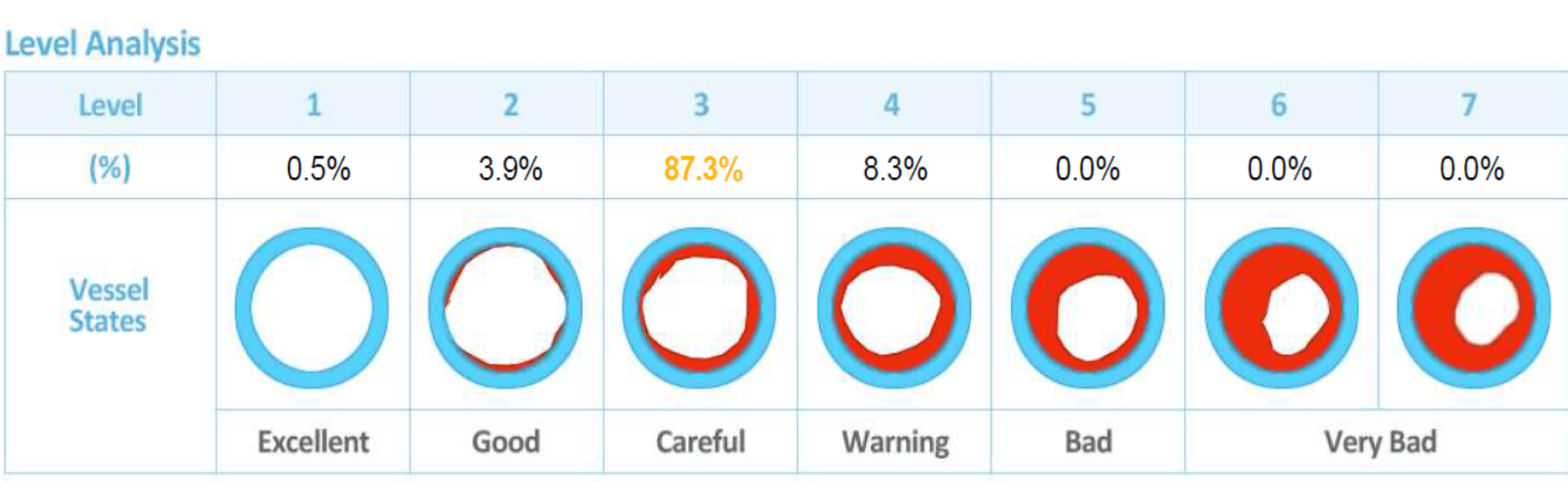
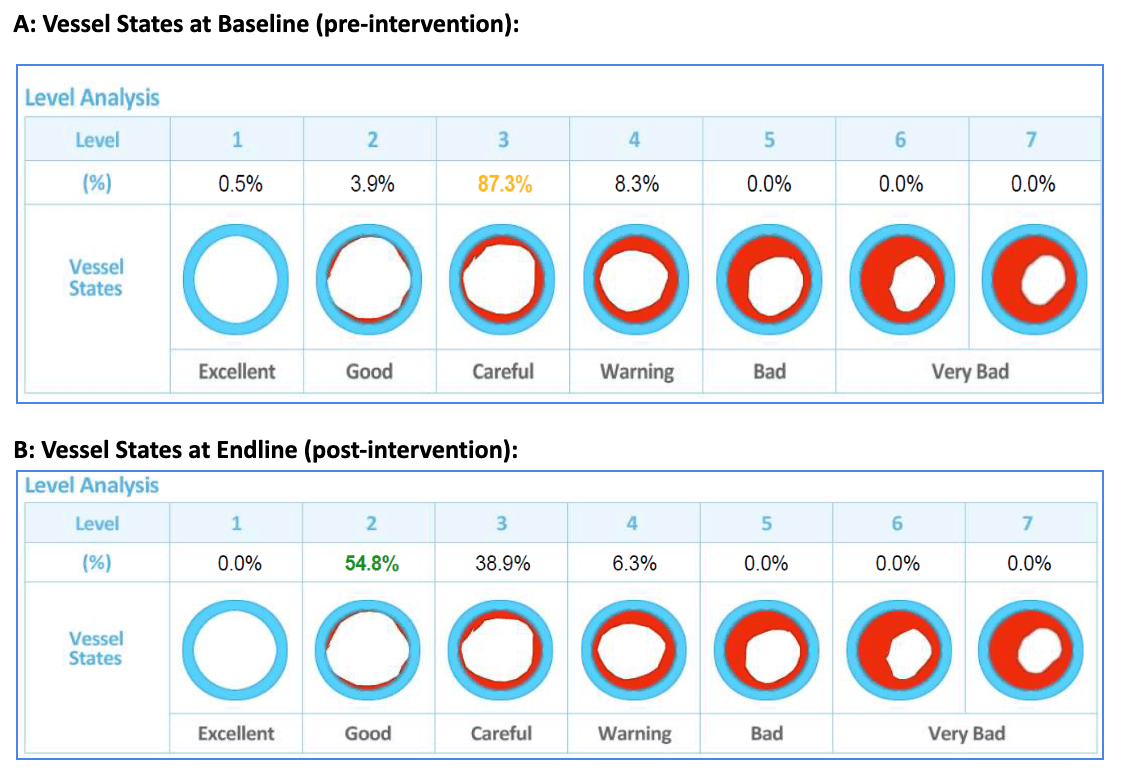
A: Vessel States at Baseline (pre intervention):
Body Text moduleB: Vessel States at Endline (post-intervention):
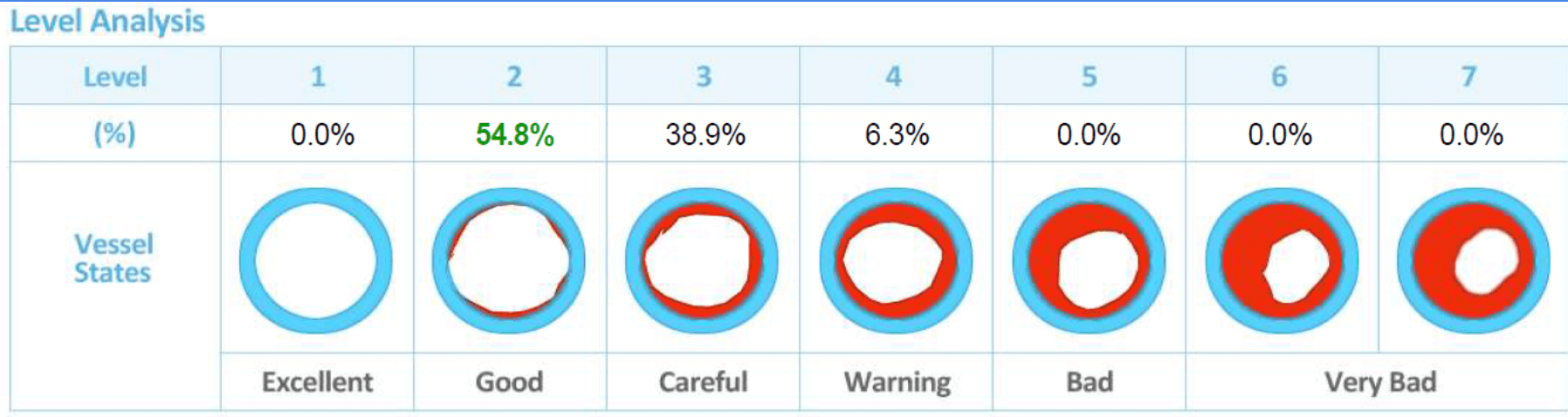
Figure 1: A graphic interpretation of waveform analysis depicts potential vessel states before (A) and after (B) RMT intervention, highlighting the percentage of vascular endothelial area in the respective state (%), and correlating it with a general description of vessel state (row below picture).
EFFECT OF RMT ON VASCULAR FUNCTION
Table 1 and figure 1 show that both arterial and peripheral elasticity improved by 10.4% and 86.3%, respectively, in response to the RMT intervention. Data on vascular elasticity were obtained by Arterial Waveform Analysis, and indicate markers for the development of vascular disease, present before the onset of symptoms. Changes in the blood pressure curve, typically describing a waveform, between systolic and end diastolic blood pressure, created by the cardiac pump, correlate with stiffness/elasticity of the arterial endothelial wall. of the arterial system normally declines with age but is also impaired in people with hypertension, coronary artery disease, heart failure, and diabetes.
Aberrant waveforms indicate reduced elasticity and circulation, increasing cardiovascular risk factors. Intervention increasing vascular compliance, such as vasodilators, cause a measurable shift in the waveform, reflecting their impact on circulation. The results observed in this case report show a similar shift in the waveform, resulting in increased elasticity scores for arterial and peripheral circulation (see table 1). Interpretation of the numerical data obtained shows that the percentage of vessels in a higher risk category (“careful”) is reduced from 87.3% to 38.9%, shifting the majority (54.8%) of vascularisation into a healthy category (“good”) (Figure 1). These improvements in vascular compliance, therefore, could contribute to slowing down the decrease of vascular elasticity as a normal process during aging, as well as to reducing cardiovascular risk [3]. Although the mechanism for RMT to modify vascular plasticity remains to be determined, supporting evidence comes from the findings that RMT reduces systolic and diastolic blood pressure in both normotensive and hypertensive adults [4,5]. Furthermore, RMT restores impaired peripheral blood flow to resting and exercising limbs in chronic heart failure patients. A proposed mechanisms here is that a reduction of peripheral vasoconstriction caused by respiratory metaboreflex [6]. More recently, RMT has also been shown to improve cardiac autonomic modulation, and cardiac and peripheral autonomic controls and cardiac output, highlighting the direct effect of RMT on cardiac function [7–9].
It is, therefore, reasonable to speculate that the improvements in vascular elasticity observed in this subject reflect a combinatorial effect of improved cardiac function and circulation, reduced flow resistance, as well as mechanisms that require further elucidation in future studies.
CONCLUSION
Sedentary lifestyles and company culture contribute to cardiovascular and cardiopulmonary changes that increase the individual risk of cardiovascular disease and deterioration of QOL. Respiratory muscle training (RMT) can be a cost- and time-effective intervention to reverse early signs of cardiac and pulmonary risk factors. This case study provides a first insight into the beneficial impact of RMT on lifestyle-mediated cardiopulmonary deterioration. These preliminary results encourage further investigation and confirmation in larger-scale studies.
References
- Shaikh S, Vishnu Vardhan GD, Gunjal S, Mahajan A, Lamuvel M. Effect of Inspiratory Muscle Training by Using Breather Device in Participants with Chronic Obstructive Pulmonary Disease (COPD). Available: http://www.ijhsr.org/IJHSR_Vol.9_Issue.4_April2019/12.pdf
- Nykvist M, Sköld M, Ferrara G, Faager G. Inspiratory muscle training in addition to physical exercise for idiopathic pulmonary fibrosis. Eur Respir J. European Respiratory Society; 2016;48: OA1518.
- Arterial Health – Overview – Long Life Cardio – Max Pulse. In: Long Life Cardio – Max Pulse [Internet]. [cited 4 Feb 2019]. Available: https://longlifecardio.com/cardio-wave-overview/
- Vranish JR, Bailey EF. Inspiratory Muscle Training Improves Sleep and Mitigates Cardiovascular Dysfunction in Obstructive Sleep Apnea. Sleep. 2016;39: 1179–1185.
- Ferreira JB, Plentz RDM, Stein C, Casali KR, Arena R, Lago PD. Inspiratory muscle training reduces blood pressure and sympathetic activity in hypertensive patients: a randomized controlled trial. Int J Cardiol. 2013;166: 61–67.
- Chiappa GR, Roseguini BT, Vieira PJC, Alves CN, Tavares A, Winkelmann ER, et al. Inspiratory muscle training improves blood flow to resting and exercising limbs in patients with chronic heart failure. J Am Coll Cardiol. 2008;51: 1663–1671.
- Feriani DJ, Coelho HJ Júnior, Scapini KB, de Moraes OA, Mostarda C, Ruberti OM, et al. Effects of inspiratory muscle exercise in the pulmonary function, autonomic modulation, and hemodynamic variables in older women with metabolic syndrome. J Exerc Rehabil. 2017;13: 218–226.
- Laohachai K, Winlaw D, Selvadurai H, Gnanappa GK, d’Udekem Y, Celermajer D, et al. Inspiratory Muscle Training Is Associated With Improved Inspiratory Muscle Strength, Resting Cardiac Output, and the Ventilatory Efficiency of Exercise in Patients With a Fontan Circulation. J Am Heart Assoc. 2017;6. doi:10.1161/JAHA.117.005750
- Mello PR, Guerra GM, Borile S, Rondon MU, Alves MJ, Negrão CE, et al. Inspiratory muscle training reduces sympathetic nervous activity and improves inspiratory muscle weakness and quality of life in patients with chronic heart failure: a clinical trial. J Cardiopulm Rehabil Prev. 2012;32: 255–261.
THANKS!
Hoping this can help me, I have sleep apnea and COPD and 4lung nodes I’ve been using the Relaxes Himalayan salt Inhaler for now and quit smoking 10 days ago, praying that this helps
Thank you for pointing out that bad lifestyle choices can have a detrimental impact on cardiopulmonary parameters and cause the weakening of the breathing muscles. My friend is struggling to breathe. I’ll advise her to get a pulmonary function test.
Looking at the original article, this is a far departure of what the website is claiming and not accurate. I am happy to discuss more. I am a speech therapist and know many people who use this device. But I have some questions about the original research.
Thank you for your comment and we make our research a high priority. I will forward this to our chief clinician to review