Poster Presentation – DYSPHAGIA RESEARCH SOCIETY, 2019, San Diego, CA
Matthew Dumican, M.S. CCC-SLP; Christopher Watts, Ph.D.
KEY FINDINGS
- In neuromuscular disease, such as Parkinson’s, activation of muscle groups for voice and swallowing may be impaired, causing dysphonia and dysphagia.
- Strengthening those muscle groups by respiratory muscle training (RMT) can improve voice and swallow function, and health-related quality of life.
- In the study presented here, activation of the hyolaryngeal muscles in response to RMT using The Breather is assessed by surface electromyograph (sEMG).
- RMT using The Breather improved muscle activation both during inspiration as well as during expiration against resistance significantly above baseline level.
- The Breather can be recommended as a useful exercise tool to maintain swallow function longer.
INTRODUCTION
Eating and drinking rank among the most necessary, but also the most enjoyable tasks in life, even more so if the experience is spiced up with exhilarating flavors and inspiring company. Being top of the hit list of life’s joys, any impact on our ability to eat and drink, for example due to disease or stroke, can have devastating consequences on physiological and mental health, and dramatically reduce the quality of life.
We spoke with Dr Chris Watts, researcher and newly appointed Dean of the Harris College of Nursing and Health Sciences at the Texas Christian University, about swallowing, speech, and how to best preserve these important physiological functions at the onset of neuromuscular diseases such as Parkinson’s. As a speech language pathologist by training, Dr Watts follows his passion as a clinician, a teacher, as well as a scholar. His academic research revolves around laryngeal function in voice and swallowing. While the muscle groups used for voice production and for swallowing may overlap, their specific roles in these distinct physiological processes differ significantly. “What happens in the larynx during swallowing, is very different than what happens in the larynx during voice production” explains Dr Watts. While the larynx has to close during swallowing to protect the lower airways, it remains open during speech production to allow for airflow through the vocal folds.
DR. WATTS EXPLAINS THE DIFFERENT FUNCTIONS THE LARYNX SERVES DURING VOICE PRODUCTION AND SWALLOWING:
Respiratory muscle training (RMT) offers a potential intervention here by increasing activity of the laryngeal muscle groups. The method of RMT follows the same principles as resistance or weight training for any other skeletal muscles. Muscles get activated by increasing their workload through resistance, which leads to an increase in muscle mass (hypertrophy) and improves muscle function. And what dumbbells are for the biceps, is a respiratory muscle trainer for the respiratory and laryngeal muscles. The Breather is a respiratory muscle trainer that provides resistance for strengthening both inspiratory and expiratory muscles, including those muscle groups used for voice and swallowing.
In a recent exploratory study conducted in the research lab of Dr Watts, the graduate researcher Matt Dumican set out to investigate the effect of the Breather on the submandibular muscles in healthy individuals. These muscles are attached to the underside of the mandible or the chin, and connect to the hyoid bone, pulling the larynx forward during swallowing to prevent food or liquid from entering the lower airways of the lungs. Dr Watts and his team were particularly interested in what happens to these muscles if you add resistance by using the Breather.
DR. WATTS DISCUSSES THE IMPORTANCE OF RESISTANCE TRAINING USING THE BREATHER FOR THE HYOLARYNGEAL MUSCLES:
DR. WATTS EXPLAINS THE STUDY DESIGN AND MAIN FINDINGS:
Figure 1: Average Hyolaryngeal Muscle Activation During Expiration Using The Breather
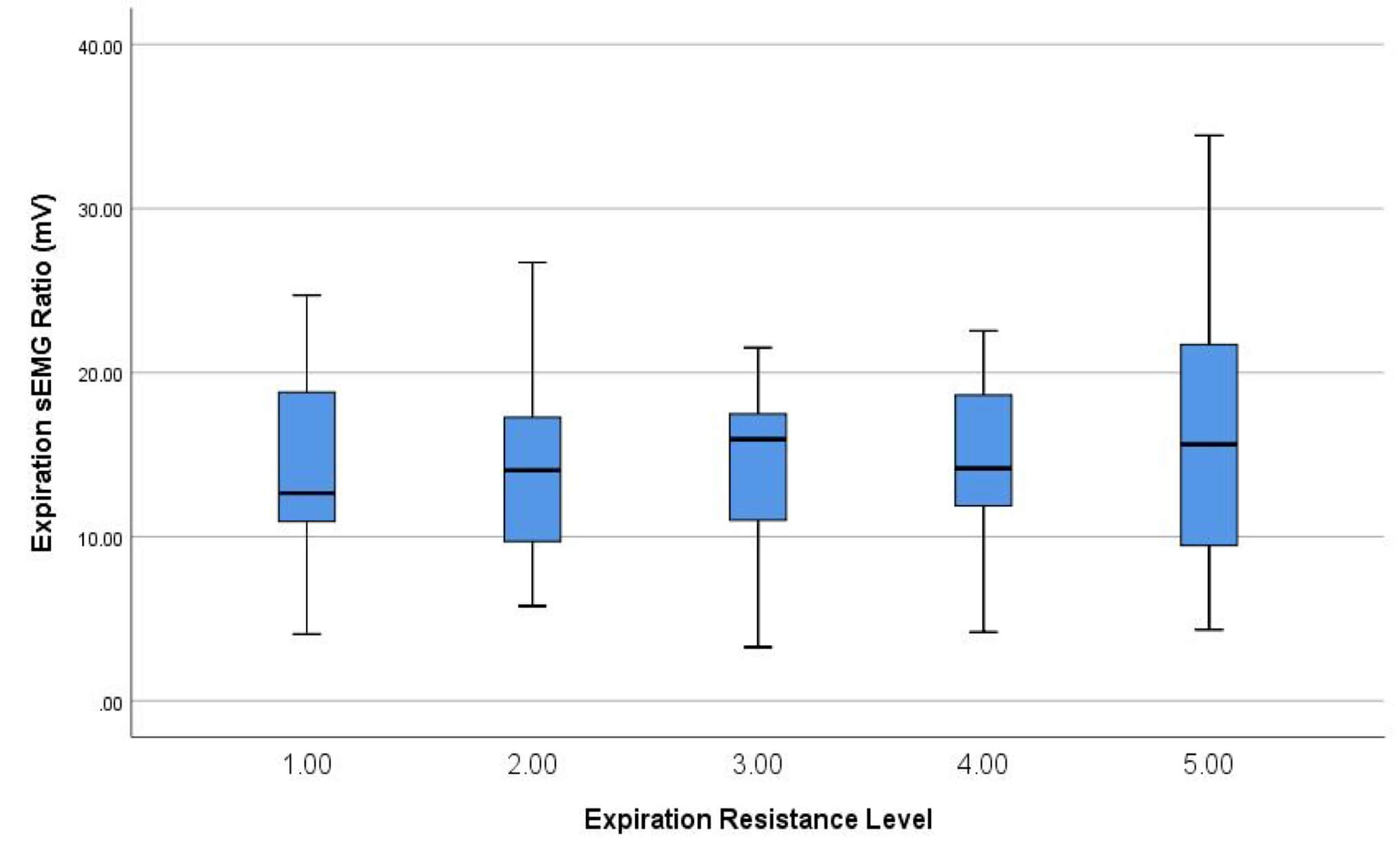
The effect size of peak muscle activation compared to baseline activity was .77 (Cohen’s d; moderate-large effect). Inspiratory tasks against resistance elicited a slightly higher effect size of .88.
Figure 2: Average Hyolaryngeal Muscle Activation During Inspiration Using The Breather
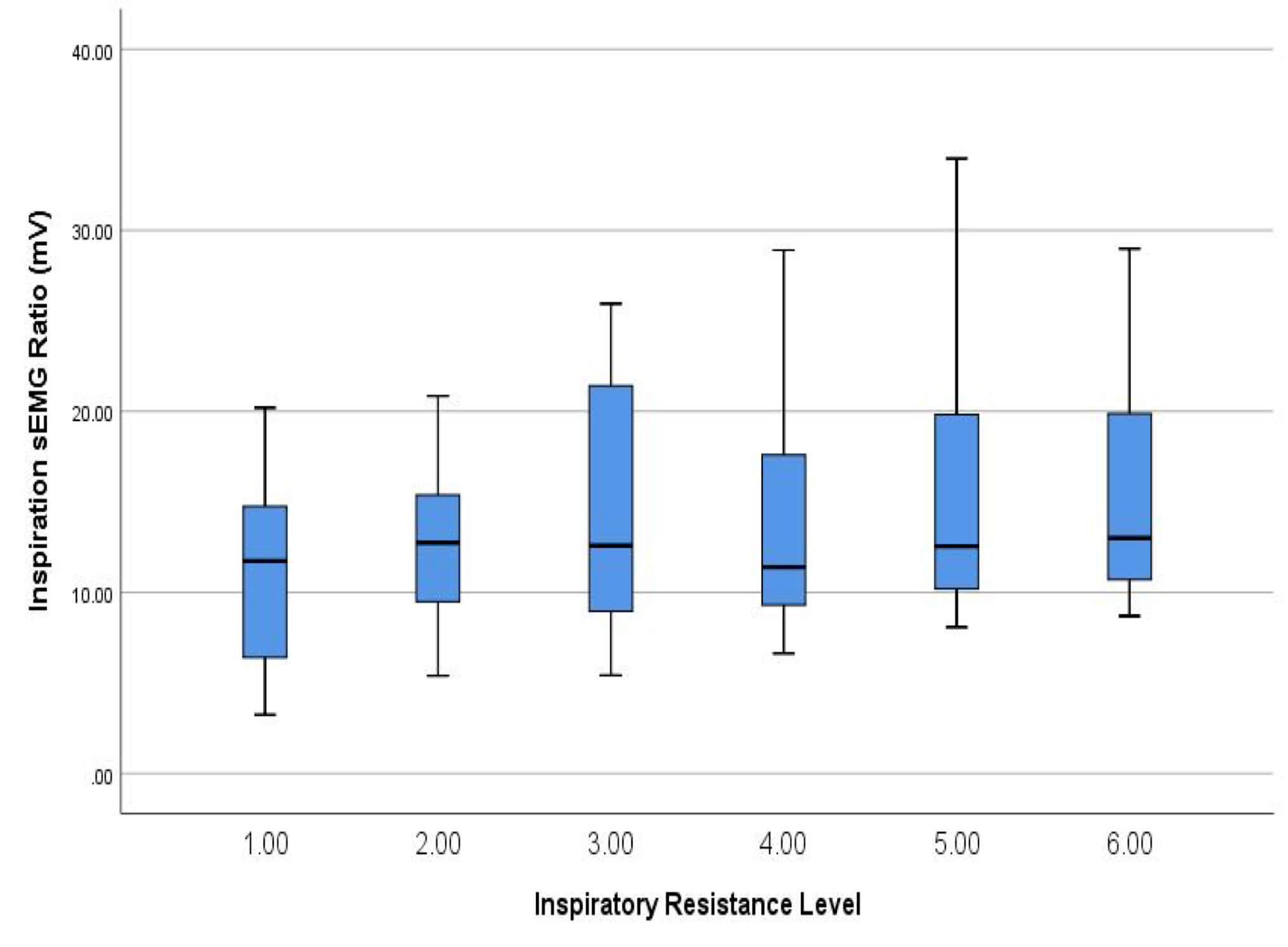
Interestingly, as shown in Figure 2, muscle activation during inspiration against resistance increased with higher settings. The Breather has 6 different resistance settings for inspiration. Muscle activation was more pronounced at the higher settings (5 and 6) than at the lower settings (1 and 2), indicating a correlation between muscle activation and training intensity.
Why a similar correlation was not observed during expiration requires further investigation, Dr Watts suggests. However, as inspiratory muscles are more accustomed to training, for example by doing exercise, higher activation levels may be possible even in people new to RMT. Expiration on the other hand is passive at rest, and relies on the natural recoil of the lung. Expiratory muscles typically take longer to train using RMT than inspiratory muscles. As none of the subjects in this study have used the Breather or similar RMT devices before, muscle response may reflect the natural strength of their respiratory muscles, with the expiratory muscles being less active than the inspiratory muscles. A second assessment after several weeks of RMT may be useful to investigate a change in activation patterns. However, these speculations need to be confirmed by future investigations.
As Dr. Watts points out, the outcomes of the study clearly show that breathing against resistance using the Breather increases activation of the hyolaryngeal muscles. The wider implications of these findings include the potential of the Breather “as a tool as part of an exercise program for these muscles in people who have an impairment that causes dysphagia.”
DR. WATTS DISCUSSES THE POTENTIAL IMPACT OF RMT ON PEOPLE WITH PARKINSON’S:
In people with neuromuscular disease, recruitment and activation of muscles involved in speech and swallow function may be impaired and decline during disease progression. The consequences of voice and swallow dysfunction can have both physiological and psychological effects. While malnutrition and an increased risk of aspiration pneumonia are linked to dysphagia and poor cough effectiveness, the social impact may be even more burdensome in people with Parkinson’s. Gathering with loved ones around a dinner table, and enjoying food, drink and conversation are an integral part of our culture, and greatly enhance our wellbeing. Not being able to fully enjoy these aspects of life due to worries about choking or the inability to make one’s voice heard can lead to stress, anxiety, social isolation and depression.
Respiratory muscle training may offer an effective therapy here, especially in the early stages, to preserve voice and swallow function as long as possible, and to maintain a longer quality of life. Dr Watts emphasizes the need for exercises, particularly for those muscles that are involved in voice and swallowing, for people with Parkinson’s, as it will help people “go for a longer time without handicap or disability related to voice and swallowing.”
Based on his findings as well as on the evidence from numerous other studies confirming the benefits of RMT in neuromuscular disease, Dr Watts paints a future scenario in which “the Breather, or other devices, in the future, we might recommend at the time of diagnosis.” In a concluding remark, Dr Watts points out that “using a device such as the Breather will do more good than it will ever do harm”, and that this is something that “people with Parkinson’s disease are looking for.”
DR. WATTS DESCRIBES A POTENTIAL FUTURE SCENARIO OF THE USE OF THE BREATHER IN PARKINSON’S:
References
Brooks, M., Mclaughlin, E., & Shields, N. (2017). Expiratory muscle strength training improves swallowing and respiratory outcomes in people with dysphagia: A systematic review. International Journal of Speech- Language Pathology, 1-12. doi:10.1080/17549507.2017.1387285
Laciuga, H., Rosenbek, J. C., Davenport, P. W., & Sapienza, C. M. (2014). Functional outcomes associated with expiratory muscle strength training: Narrative review. Journal of Rehabilitation Research and
Development, 51(4), 535-546. doi:10.1682/jrrd.2013.03.0076
Wheeler-Hegland, K. M., Rosenbek, J. C., & Sapienza, C. M. (2008). Submental sEMG and Hyoid Movement During Mendelsohn Maneuver, Effortful Swallow, and Expiratory Muscle Strength Training. Journal of Speech Language and Hearing Research, 51(5), 1072. doi:10.1044/1092-4388(2008/07-0016)
Wheeler, K. M., Chiara, T., & Sapienza, C. M. (2007). Surface Electromyographic Activity of the Submental Muscles During Swallow and Expiratory Pressure Threshold Training Tasks. Dysphagia, 22(2), 108-116. doi:10.1007/s00455-006-9061-4
0 Comments