CLINICAL CONTEXT AND KEY FINDINGS
- Home-based COPD management, as provided by certified home-health providers, represents a cornerstone of patient care.
- Respiratory muscle training (RMT) reduces symptoms of COPD and improves underlying respiratory muscle weakness, and may be a beneficial adjunct of standard of care treatment plans.
- This 4-week pilot study shows that RMT in combination with a standard of care home-based COPD management program can improve pulmonary and speech functions.
- The pilot was designed by clinical staff members of Amedisys, Inc and PN Medical, Inc. It was administered at Amedisys facilities by their therapists. The patients were all issued RMT devices named, The Breather from PN Medical and adhered to Amedisys’s standardized COPD home-based standard of care plan.
INTRODUCTION
COPD is a progressive obstructive disorder, affecting more than 15 million people in the US. The cardinal symptoms of COPD are dyspnea and limited exercise tolerance, which are to a significant extent caused by respiratory muscle weakness. Approximately 19% of patients with moderate to severe COPD experience acute exacerbations, which are critical episodes of the disease requiring immediate care and hospitalization. In high-income countries, COPD is the third leading cause of death, causing 3.8% of all deaths [1][2][4][3]. Treatment strategies for COPD include bronchodilators and rehabilitation to improve exercise capacity. However, the underlying respiratory muscle weakness is not addressed by current pharmacological or rehabilitative COPD management approaches.
Due to the progressive course of COPD and its burden on the health system, long-term self-management of COPD patients is critical. While patients usually experience in-hospital care during the acute stage of the disease, management of the chronic stages of COPD is often neglected, contributing to rapid progression and worsening of symptoms. Institutionalized pulmonary rehabilitation is an effective method to improve symptoms of COPD and to increase exercise capacity and QOL. However, pulmonary rehabilitation is only available to approximately 2% of eligible COPD patients [4].
Home-based exercise regimes offer a valuable alternative, and have proven to be as effective as hospital-based or outpatient pulmonary rehabilitation [5–7]. Home-based COPD management interventions such as patient activation, active monitoring of adherence, care coordination and medical management reduce sedentary behavior and It is made available under a CC-BY-ND 4.0 International license. (which was not peer-reviewed) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. bioRxiv preprint first posted online Jan. 17, 2019; doi: http://dx.doi.org/10.1101/523746. The copyright holder for this preprint increase physical activity levels. Furthermore, home-based COPD management reduces healthcare utilization, acute care hospitalization days, and mortality [8,9].
Optimal management of COPD patients includes pulmonary rehabilitation and counter measures to decrease the respiratory muscle weakness underlying the disease. Respiratory muscle training (RMT) is a drug-free therapeutic method that triggers respiratory muscle hypertrophy and improved functioning by loading the muscles during training. In resistive RMT, the air flow generated during the breathing cycle is forced through different sized apertures, adding resistance to the flow path, thereby loading the entire pressure curve of the breath flow. Intensity of RMT and workload of on the respiratory muscles is increased with decreasing aperture size [10].
This pilot study investigated the effectiveness of RMT on clinical parameters of COPD patients in a home-health setting, with the aim of exploring the potential of home-based RMT management to emulate the benefits of institutionalized pulmonary rehabilitation.
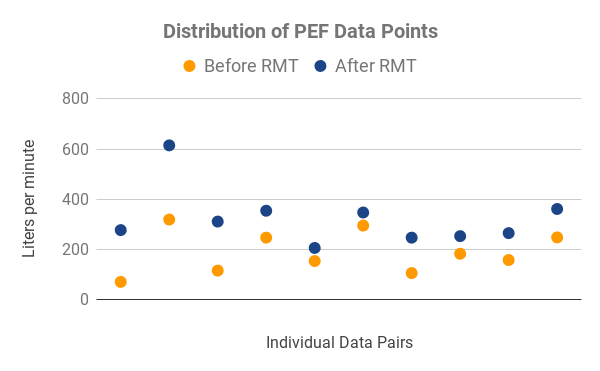
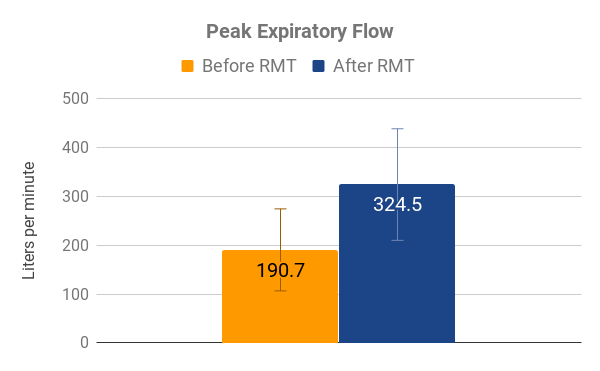
Figure 1: Distribution of PEF data points (left panel) show the individual collected data pairs. Orange dots indicate the values collected at the beginning of the study (pre-RMT), blue dots in direct vertical line above the orange dot indicate measurement from the same subject at the end of the study period (post-RMT), in liters per minute. Peak expiratory flow (PEF, right panel) shows average PEF pre-RMT (orange) and post-RMT (blue) values, n=11. Error bars indicate standard deviation, P-Value<0.001 (paired t-test).
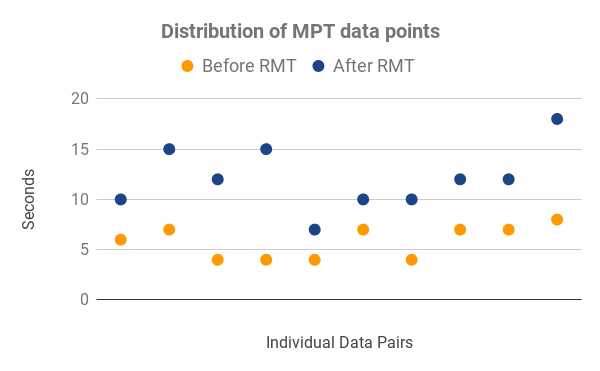
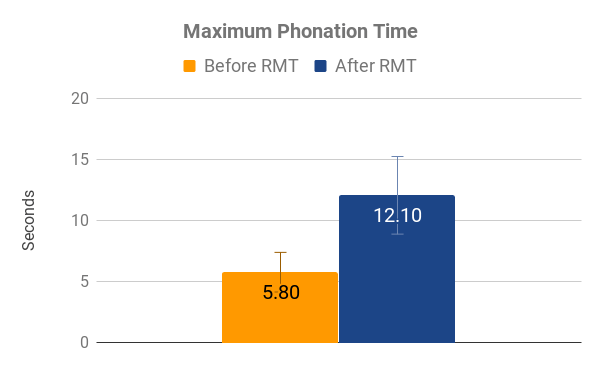
Figure 2: Distribution of MPT data points (left panel) show the individual collected data pairs. Orange dots indicate the values collected at the beginning of the study (pre-RMT), blue dots in direct vertical line above the orange dot indicate measurement from the same subject at the end of the study period (post-RMT), in seconds. Maximum phonation time (MPT, right panel) shows average MPT pre-RMT (orange) and post-RMT (blue), n=11. Error bars indicate standard deviation, P-Value<0.001 (paired t-test).
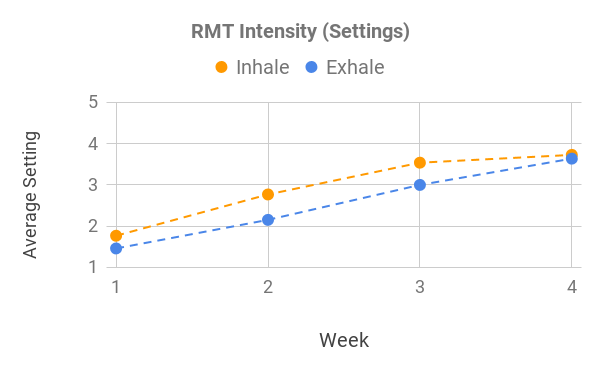
Figure 3: Increase of Average RMT Intensity Outlined by Increase in Settings. Orange line indicates the average increase in inhale settings (minimum: 1, maximum: 6) over the study period (4 weeks), blue line indicates the average increase in exhale settings (minimum: 1, maximum:5) over the study period.

0 Comments